Greetings fellow plebs & peasants,
I started working on this post with the intention of showing only the postive uses of biotech. Contrary to how some previous posts on these matters ma have come across, I am not opposed to the prospects of what biotech research can eventually lead to. My issue is coercing/forcing any of these treatments on people (such as mRNA mandates) especially when they are still in trial phases. If a person wants to be a test subject, and is given full disclosure as to all known ill effects from a treatment, by all means, a person has that right. Another issue I have is the highly questionable ethics involved in many dystopic applications of the technology. There are some things that just because it can be done, does not mean it should be done. And rabbit holes being rabbit holes, my research for this took a wierd turn and found some creepy ass shit. So with that in mind, this post begins with a couple heart warming successes in this field. A young girl with Luekemia given a new lease on life thanks to gene-editing, and brain/computer intefaces for the disabled (who is in any postion to tell a paralyzed person he or she should not give anythig a chance to acheive even a small amount of self-sufficiency?). In contrast, and while still more conceptual than anything else, a horror show straight out of the Matrix and/or Brave New World and some new Dr. Moreau-esque gene spicing. I think this presents a clear cut case that biotech is merely a tool/technology, that like all others, is merely neutral. It is who wields it, and to what ends, can it be considered good or bad.
- jw
The Good:
…Bio-technology
Ain't what's so bad…
Source: The Debrief
Brain-Machine Interface Allows Wheelchair to Navigate a Cluttered Room With ‘Mind Control’
November 21, 2022
A new brain-machine interface (BMI) lets patients navigate a wheelchair through a crowded room using only the power of mind control. The researchers behind the new BMI say it takes some training to become proficient, and not all patients were successful. The researchers also point out that their BMI mind control-driven wheelchair uses a non-invasive headband to interpret brain signals instead of a more-invasive implant like the more well-known Neuralink championed by Elon Musk.
Brain Machine Interfaces Breaking Barriers for the Disabled
While science fiction fans may envision using BMI’s to change TV channels, surf the web, drive their car, or fly a personalized flying saucer, the most promising benefits may come to users with disabilities who struggle to perform everyday tasks. Last year, The Debrief reported on a movement-impaired patient at Johns Hopkins University who used an implanted BMI to cut up a Twinkie and feed it to himself, an act the patient described as “cool.”
More recently, Elon Musk’s Neuralink made headlines by demonstrating how a monkey with implanted BMIs was able to play the rudimentary video game, Pong. Still, implanted BMIs come with a number of risks and challenges, not to mention the cost associated with BMIs that demonstrate this level of sophistication. Now, a group of researchers from the University of Texas at Austin has demonstrated a non-invasive BMI that offered the majority of test subjects the ability to navigate their powered wheelchairs through a cluttered room with a very high degree of accuracy.
Mind Control BMI drives wheelchair Without Implantation
First, the researchers recruited three tetraplegic people. Each volunteer underwent training sessions three times a week for anywhere from 2 months to five months, depending on the level of success. This involved wearing a full skull cap with was able to read brain signals using standard electroencephalography (EEG). This is critically important, as most BMI are implanted directly into the human brain.
The EEG skullcap was specifically designed to read the patient’s mind and converted specific signals into commands to turn the chair left or right. For this study, the volunteers were told to think about moving both of their hands if they wanted to turn left or moving both of their feet if they wanted to turn right. This method is also significant because in most tetraplegic people, the part of their brain that engages their hands or feet to move is still working properly, and their lack of mobility is due to other factors.
All three volunteers performed similarly in the first training session, with the wheelchair’s directional control correlating to the user’s thoughts somewhere between 43% and 55% of the time. However, two of the three participants saw significant advancements as the training sessions progressed. For one, this meant achieving around 95% correlation between their desired direction and the direction interpreted by the computer driving the chair, while another topped out at 98% accuracy about halfway through the series of training sessions.
Conversely, the third participant saw only a very small increase in accuracy after their initial sessions and experienced no improvement over the course of the study. The study authors believe the difference in success was rooted in the brain’s ability to offer a strongly differentiated signal between the “go left” commands and the “go right” commands.
“We see from the EEG results that the (successful) subject has consolidated a skill of modulating different parts of their brains to generate a pattern for ‘go left’ and a different pattern for ‘go right,’” says José del R. Millán, the study’s corresponding author at The University of Texas at Austin, in a press release.
Specifically, Millán and his team believe there is a “cortical reorganization” that occurred during the participants’ learning process that allowed them to improve their mind control of the wheelchair with more training.
“It seems that for someone to acquire good brain-machine interface control that allows them to perform relatively complex daily activity like driving the wheelchair in a natural environment, it requires some neuroplastic reorganization in our cortex,” he explained.
By the end of the training sessions, all three participants used their new min control wheelchairs to maneuver through a cluttered environment using only the power of their thoughts. As expected, the two subjects who were successful in the training process were able to complete the obstacle course, while the patient who showed little improvement was unable to complete the challenge.
Improving the Mind Control BMI, so it Works for Everyone
Published in the journal iScience, the new study offers significant hope for people suffering from limited mobility, especially those confined to a wheelchair. And the researchers note the success of such a system requires learning from both their algorithm and the user.
“We show that mutual learning of both the user and the brain-machine interface algorithm are both important for users to successfully operate such wheelchairs,” says Millán.
Plus, Millán notes, the ability to achieve such a high level of accuracy and control using only an external EEG and without an implanted BMI is a significant step in reducing complications, cost, and complexity of these systems for general use.
“Our research highlights a potential pathway for improved clinical translation of non-invasive brain-machine interface technology,” he explains.
Next, the researchers say they want to take a deeper look at the patient who was unable to improve their control of the device in hopes of figuring out what went wrong and where they can improve the training process. Then, they hope to help improve the technology for those who were able to use mind control to maneuver their wheelchairs so it can be made available to a wider range of people who lack mobility.
Source: Freethink
Australian man uses brain implant to send texts from his iPad
He clicked letters on the screen by thinking about tapping his foot.
November 12, 2022
An Australian man with ALS has used a brain-computer interface (BCI) called the Stentrode to send text messages from his iPad — marking the first time anyone has used the unique implant to control an Apple device.
“What’s really exciting about this project … is that they’ve done something really innovative and connected it into something that’s standard,” Gillian Hayes, a professor of informatics at UC Irvine, who isn’t involved with the experiment, told media startup Semafor.
The challenge
Amyotrophic lateral sclerosis (ALS) is a rare neurological disorder that kills the neurons that govern voluntary movement and muscle control.
Initial symptoms can include twitching or muscle stiffness, but as the disease progresses, a person can lose their ability to move, speak, or even breathe. There is still no way to stop this progression, and the average survival time after an ALS diagnosis is just 2 to 5 years.
Most people with ALS experience speech difficulties, and in the disease’s later stages, they may lose their ability to speak altogether. If their hands are also affected, they may need to rely on tech that tracks small movements, such as blinking or cheek twitches, to communicate.
In really severe cases, a person with ALS might not be able to move any muscles, even the ones that control blinking. They will be aware of the world around them, but unable to communicate their thoughts — with devastating impact on their mental health and quality of life.
As ALS progresses, a person can lose their ability to move, speak, or even breathe.
Mind readers
BCIs — devices that translate brain activity into commands for computers — are emerging as a way for people with ALS and other paralyzing conditions to communicate with the world.
These devices might allow a patient to move a cursor around a computer screen by thinking about moving a joystick with their hand, for example, or type text on a screen by thinking about handwriting each letter in a word.
“In spite of muscles that are paralyzed, the actions that those muscles are trying to convey can be routed out through signals in the brain,” explained Douglas Weber, a professor of mechanical engineering and neuroscience at Carnegie Mellon University.
“Our thoughts drive the actions of our muscles and in the absence of muscles that work, those messages can be conveyed through sensors that are placed in or around the brain to pick up those messages,” he continued.

For now, though, these devices are mostly confined to one-off experiments, stuck in labs and universities. If you or someone you loved wanted to get one, you couldn’t just buy it.
They also tend to require invasive surgery to implant the electrodes. This approach isn’t just risky — it puts a relatively short expiration date on the device. Scar tissue tends to develop around the implant, which weakens the signal over time until it becomes useless.
The Stentrode
In 2021, New York-based tech company Synchron received FDA approval to launch a clinical trial of its in-development BCI, the Stentrode — positioning it as a frontrunner in the race to create a commercial BCI.
The Stentrode is a matchstick-sized implant, shaped like a mesh tube, and it’s designed to sit inside the blood vessel that runs down the center of the brain — rather than in the brain tissue itself.
“The blood vessels let you access all areas of the brain, superficial and deep,” Tom Oxley, Synchron’s co-founder and CEO, told Fierce Biotech in 2021.
To implant a Stentrode, surgeons make a small incision in a patient’s neck, insert the tech into the jugular vein, and then push it into place. The mesh then expands so that its 16 tiny electrodes press against the interior wall of the blood vessel.
A wire runs from the Stentrode down the body to the patient’s chest, where a small device called the “Synchron Switch” is implanted just under the skin. That device wirelessly transmits brain activity data to an external receiver.
The external receiver uses a machine learning algorithm to translate the brain data into commands that can be sent to a laptop or other device.
After promising animal studies, Synchron launched its first clinical trial of the Stentrode in Australia in 2019. The US trial just launched in 2022, and six people have now undergone the minimally invasive procedure to implant a Stentrode — and the results are incredible.
“[I]t gives you back the ability to be independent,” Philip O’Keefe, an ALS patient participating in the Australian trial, told the Economist. “There is no doubt from my perspective being involved in this gave me a reason to live.”
On November 4, Semafor reported that Rodney Gorham, another Australian trial participant with ALS, had become the first person to use one of Synchron’s BCIs to send text messages from an Apple device, clicking letters on an iPad screen by thinking about tapping his foot.
“We’re excited about iOS and Apple products because they’re so ubiquitous,” Oxley told Semafor.
The Synchron advantage
Most in-development BCIs feature electrode arrays implanted into brain tissue via open-brain surgery — that procedure requires the skill of an expert neurosurgeon and a standard 3 to 7 day hospital stay for patients.
Patients can go home as soon as 48 hours after getting a Stentrode implanted, though, and Oxley told Semafor that the skills needed for the procedure — threading a wire through a vein — are “commonplace,” which could make it more accessible to more patients in more places.
Scar tissue can form around a traditional electrode array, too, affecting a BCI’s efficacy over time — a completely paralyzed ALS patient who could once spell sentences on a screen with his BCI was limited to answering yes or no questions three years after his implantation surgery.
The placement of Synchron’s implant eliminates the problem of scar tissue impairing performance — some researchers believe the signal quality might actually improve over time as the device becomes more stable in its blood vessel.
It’s too soon to say whether that’s the case, but none of the participants in Synchron’s trials have experienced serious adverse effects from the devices so far. Four of them have had their implants for more than a year without problems.
If the US trial goes well, Synchron believes it could have a commercial device approved as soon as 2024 — finally bringing BCIs out of labs and into the homes of people with ALS and other paralysis-causing conditions.
Source: Great Ormond Street Hospital
GOSH patient receives world-first treatment for her 'incurable' T-cell leukaemia
December 11, 2022
In May 2022, Alyssa, 13 from Leicester, became the first reported patient in the world to receive base-edited T-cells at Great Ormond Street Hospital for Children (GOSH), in collaboration with the UCL Great Ormond Street Institute of Child Health (UCL GOS ICH), to treat her ‘incurable’ T cell leukaemia.
In 2021, Alyssa was diagnosed with T-cell acute lymphoblastic leukaemia (T-ALL) and received all current conventional therapies for her cancer, including chemotherapy and a bone marrow transplant. Unfortunately her disease came back and there were no further treatment options available as part of routine care.
Alyssa was the first patient to be enrolled onto a new clinical trial and in May she was admitted to the Bone Marrow Transplant (BMT) Unit at GOSH, to receive genetically modified CAR T-cells that originally came from a healthy donor. These cells had been edited using new base-editing technology to allow them to hunt down and kill the cancerous T-cells without attacking each other.
Just 28 days later, she was in remission and went on the receive a second bone marrow transplant to restore her immune system. Now, six-months post-BMT, she is doing well at home recovering with her family and continues her post-BMT follow-up at GOSH.
Base editing and CAR T-cell therapy
An animated explainer video about base editing. Illustrated by Dr Maryam Clark (as part of an NIHR GOSH BRC Research Communications Internship), edited by Maisie Hardy.
It has been more difficult to treat T-cell leukaemia with traditional CAR T-cell therapy because T-cells designed to recognise and attack cancerous T-cells also end up killing each other during the manufacturing process before they can be given as a treatment.
Teams at GOSH and the UCL GOS ICH have therefore been working, using a new genome editing technique called base-editing, to create a new type of CAR T-cell therapy that is able to attack cancerous T-cells. Base editing works by chemically converting single letters of the DNA code (single nucleotide bases) to change the T-cells.
The team used the technique to make multiple changes to healthy donor T-cells, arranged by the Anthony Nolan registry, that have meant cells do not need to be collected from the patient:
Changing the donor T-cells so that they aren't attacked by the patients own immune system
Removing a ‘flag’ on the modified T-cells that means they won't attack each other before they can be used as a treatment
Removing a second ‘flag’ that means the cells are invisible to other cancer treatments
Adding a way for the modified cells to now recognise and attack cancerous T-cells
The result is edited CAR T-cells that can be given to the patient so that they rapidly find and destroy T-cells in the body, including leukemic T-cells. If successful, the patient then receives a bone marrow transplant to restore their depleted immune system.
This is a great demonstration of how, with expert teams and infrastructure, we can link cutting edge technologies in the lab with real results in the hospital for patients. It’s our most sophisticated cell engineering so far and paves the way for other new treatments and ultimately better futures for sick children. We have a unique and special environment here at GOSH and the UCL GOS ICH that allows us to rapidly scale up new technologies and we’re looking forward to continuing our research and bringing it to the patients who need it most.
Professor Waseem Qasim, Professor of Cell and Gene Therapy at UCL GOS ICH and Consultant Immunologist at GOSH
Alyssa’s story
Since Alyssa got sick with her leukaemia in May last year, she never achieved a complete remission. Not with chemotherapy and not after her first bone marrow transplant. Only after she received her CD7 CAR-T cell therapy and a second bone marrow transplant in GOSH she has become leukaemia free. This is quite remarkable, although it is still a preliminary result, which needs to be monitored and confirmed over the next few months. The entire team here at GOSH are extremely happy for Alyssa and her family and it’s been a privilege to work with them over the past few months. We have been very impressed by how brave she is and nothing makes me happier than seeing her outside the hospital, going back to a more normal type of life.
Dr Robert Chiesa, Consultant in Bone Marrow Transplant and CAR T-cell therapy at GOSH
Alyssa was diagnosed with T-cell leukaemia in May 2021, after a long period of what the family thought were colds, viruses and general tiredness.
While she was treated in Hospitals in Leicester and Sheffield with standard therapies - chemotherapy and a bone marrow transplant - unfortunately the teams were unable to get her cancer under control and into remission.
With the only other option as palliative care, Alyssa and her family extensively discussed this clinical trial with the BMT and CAR T-cell therapy experts and haematology service at GOSH and undertook the decision to be the first to try an experimental treatment for her leukaemia.
Once I do it, people will know what they need to do, one way or another, so doing this will help people – of course I’m going to do it.
Alyssa, 13
Alyssa is the first patient in the world reported to have received a base-edited cell therapy and is currently at home recovering from her treatment. Alyssa and her family are feeling positive that the leukaemia is now undetectable, but know she will need to be monitored closely for some time.
Kiona, Alyssa’s mum said:
“The doctors have said the first six months are the most important and we don’t want to get too cavalier but we kept thinking ‘If they can just get rid of it, just once, she’ll be ok.’ And maybe we’ll be right.”
“Alyssa is very mature and you can forget she is just a child but hopefully this can prove the research works and they can offer it to more children - all of this needs to have been for something. It just feels so senseless. Now we are trying to live between appointments. Alyssa wants to go back to school and that could be a reality soon. She’s already teasing her brother as he has had to go back for Autumn term.”
We’re on a strange cloud nine to be honest – it’s amazing to be home
Kiona, Alyssa’s mum
Alyssa is the first patient to receive this treatment during the trial but the team are aiming to recruit up to ten patients with T-cell leukaemia who have exhausted all other treatment options. The Bone Marrow Transplant (BMT) and CAR T-cell therapy teams at GOSH hope that, if the trial is successful, the treatment could be offered to children earlier in their treatment journey. They are also hoping that the technique could be an option for other types of leukaemia.
Support for research
This trial was funded by the Medical Research Council. Support for the broader research programme also comes from Wellcome, Blood Cancer UK and the National Institute of Health and Care Research (NIHR) and the NIHR GOSH Biomedical Research Centre.
Alyssa’s care was led by the BMT and CAR-T research and clinical team at GOSH, with contribution from doctors, nurses and allied professionals.
The cells were manufactured as part of a long-standing research programme led by Professor Waseem Qasim at UCL Great Ormond Street Institute of Child Health, who is also an Honorary Consultant at GOSH.
Thanks to early funding from Great Ormond Street Hospital Children’s Charity (GOSH Charity), Professor Qasim has been a pioneer in developing new CAR T-cell treatments using innovative gene editing techniques and is based at the Zayed Centre for Research into Rare Disease in Children, a partnership between GOSH and UCL GOS ICH.
The research team wish to thank Anthony Nolan for providing the donor T-cells and all of the donors who donate to the register.
At GOSH, we are also developing plans for a new clinical building dedicated to caring for children and young people from across the UK with rare and difficult-to-treat cancers. This will mean our advances in research, care and treatments will be delivered in a specially designed centre focused on the needs of children and their families and on making it easier for us to go even further and faster in developing new and kinder treatments for children with cancer.
This trial is only accepting patients eligible for NHS care. Any patients eligible to receive treatment under the NHS and interested in this trial should approach their specialist healthcare provider.
Source: Nanowerk News
Microrobots could unblock medical devices in the body
(Nanowerk News) Swarms of microrobots injected into the human body could unblock internal medical devices and avoid the need for further surgery, according to new research from the University of Essex. The study is the first-time scientists have developed magnetic microrobotics to remove deposits in shunts – common internal medical devices used to treat a variety of conditions by draining excess fluid from organs. Shunts are prone to malfunctioning, often caused by blockages due to a build-up of sediment. The sediment not only narrows and obstructs liquid passing through the shunt, but it also affects the shunt’s flexibility. This leads to patients needing repeated, invasive surgeries throughout their lives either to replace the shunt or use a catheter to remove the blockage. However, this new research, led by microrobotics expert Dr Ali Hoshiar, from Essex’s School of Computer Science and Electronic Engineering, has shown there could be a wireless, non-invasive alternative to clearing the blockage in a shunt. Published in the IEEE Transaction on Biomedical Engineering journal ("A novel non-invasive intervention for removing occlusions from shunts using an abrading magnetic microswarm"), Dr Hoshiar and his team have shown that a swarm of hundreds of microrobots – made of nano size magnetic nanoparticles – injected into the shunt could remove the sediment instead. “Once the magnetic microrobots are injected into the shunt they can be moved along the tube to the affected area using a magnetic field, generated by a powerful magnet on the body’s surface,” explained Dr Hoshiar. “The swarm of microrobots can then be moved so they scrape away the sediment, clearing the tube. “The non-invasive nature of this method is a considerable advantage to existing methods as it will potentially eliminate the risk of surgery and a surgery-related infection, thereby decreasing recovery time.” With each microrobot smaller than the width of a human hair, once the swarm has done its job, it can either be guided to the stomach via a magnetic field or bodily fluid, so they leave the body naturally. Because the microrobots have very high biocompatibility they will not cause toxicity. The research also found a direct relation between the strength of the magnetic field and the success of scraping away the sediment in the shunt. This is the first proof-of-concept experiment using microswarms for opening a blockage in a shunt. The next stage of this research is to work with clinicians to carry out trials. The researchers are also looking at how the concept can be used to other applications.
The Horror Show:
…Bio-technology
Ain't what's so bad
Like all technology
It's in the wrong hands
Cut-throat corporations
Don't give a damn
When lots of people die
From what they've made.
...From the Social Predestination Room the escalators went rumbling down into the basement, and there, in the crimson darkness, stewing warm on their cushion of peritoneum and gorged with blood-surrogate and hormones, the foetuses grew and grew or, poisoned, languished into a stunted Epsilonhood. With a faint hum and rattle the moving racks crawled imperceptibly through the weeks and the recapitulated aeons to where, in the Decanting Room, the newly-unbottled babes uttered their first yell of horror and amazement.
- Brave New World, by Aldous Huxley.
Note:
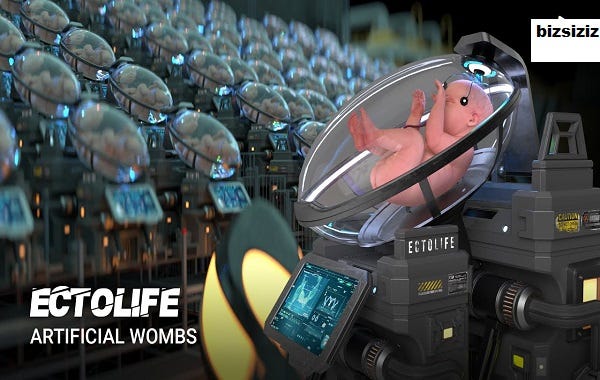
From all appearances this EctoLife is NOT an actual company. This is more a conceptual marketing campaign, although in researching for this post, I did come across a lecture/presentation (follows EtchLife article) of actual early research into this madness.
- jw
Source: Bizsiziz.com
EctoLife: Concept Unveiled for the World’s First Artificial Womb Facility
EctoLife: Concept Unveiled for the World’s First Artificial Womb Facility
In late 2021, Elon Musk tweeted his fears about the end of humanity. “We should be much more worried about population collapse….If there aren’t enough people for Earth, then there definitely won’t be enough for Mars,” he opined. Musk’s statements brought the world’s falling birthrate to the forefront of social consciousness.
For nearly a century, fertility rates have been decreasing globally. The result is what scientists are describing as a “worldwide infertility crisis.” But there’s a solution looming on the horizon — artificial wombs.
In 2017, scientists created a “BioBag” that functioned as an artificial womb, and they used it to grow a baby lamb. Now, a new concept has been unveiled showing how the same could be done for humans. In recently released footage, Hashem Al-Ghaili shows what childbirth might look like tomorrow. Specifically, he created an artificial womb facility named EctoLife.
Its purpose? In an exclusive interview with Science and Stuff, Al-Ghaili says he thinks the EctoLife concept could one day supplant traditional birth. In so doing, he said society would finally be able to meet the needs of parents who are “tired of waiting for a response from an adoption agency” and those who are “worried about pregnancy complications.” But most importantly, he says EctoLife could allow us to confront the infertility crisis head-on.
Our need for a new form of birth
Currently, the World Health Organization estimates that 15% of reproductive-aged couples worldwide are affected by infertility. Indeed, over the last 70 years, fertility rates worldwide have decreased by a staggering 50%. Reasons for this decline include (among other things) women’s increased education, increases in employment, the high cost of raising children, and a drop in global sperm count. 23 countries are already at risk, with Japan, Spain, Portugal, Thailand, and South Korea at the forefront of the crisis.
In the U.S., infertility statistics are likewise sobering:
1 in 8 American couples has issues with fertility.
12-15% of all couples are unable to conceive after a year of unprotected sex.
10% of all couples are unable to conceive after two years of unprotected sex.
33% of Americans have turned to fertility treatments or know someone who has.
Replying to Musk’s tweet, the tech investor Sahil Lavingia wrote, “We should be investing in technology that makes having kids much faster/easier/cheaper/more accessible. Synthetic wombs, etc.” And that is exactly what Al-Ghaili was thinking when he came up with the design for EctoLife. Al-Ghaili told Science and Stuff that he was inspired to create the concept of EctoLife in order to further “the discussion around a technology that shouldn’t be ignored.”
According to Al-Ghaili, the artificial womb concept of EctoLife would be life-changing for many who struggle to conceive. “It’s a perfect solution for women who [have] had their uterus surgically removed due to cancer or other complications. It could also help solve issues that stem from low sperm count,” Al-Ghaili said enthusiastically, adding that the EctoLife concept (or technologies like it) “could ultimately make miscarriage a thing of the past.”
Science fiction becomes reality.
Synthetic wombs might sound like the stuff of science fiction, but they follow in a long line of advancements in reproductive technology. On July 25, 1978, a baby girl named Louise Brown was born at Oldham and District General Hospital in Manchester, England. What made her birth memorable was that Louise was conceived in a petri dish, and she is the first baby conceived through in vitro fertilization (IVF).
Louise’s mother had a mature egg removed from one of her ovaries, and it was combined with Louise’s father’s sperm. The resulting embryo was then transferred to Mrs. Brown’s uterus. Nine months later, Louise was born. The Browns went on to conceive a second daughter, Natalie, also through IVF. In May 1999, Natalie made history when she became the first IVF baby to give birth to a child of her own. In December 2006, Louise followed suit, delivering a healthy baby boy.
Today, more than 8 million children are conceived through IVF annually.
The 2017 BioBag was an enormous breakthrough in artificial womb technology. The scientists behind the work grew eight fetal lambs for 105 to 120 days — about equivalent to human fetuses at 22 to 24 weeks of gestation. Then in March 2021, another milestone was achieved. Israeli scientists were able to grow mouse embryos for up to eleven days inside artificial wombs. What is remarkable about that achievement is that 11 days is over half of the full mouse gestational term.
Al-Ghaili says the EctoLife concept is just the logical next step. And he’s not the only one who thinks so.
“It seems probable that we are only several years away from testing [aritfical wombs] on human subjects,” Social Ethics and Policy Academic Elizabeth Chloe Romanis wrote in the BMJ’s Journal Of Medical Ethics. Meanwhile, Dr. Carlo Bulletti, Associate Professor at Yale University’s Obstetrics, Gynecology, and Reproductive Science Department, thinks that a fully functioning artificial womb could be realized within the next 10 years.
Source: M.I.T. News
New CRISPR-based tool inserts large DNA sequences at desired sites in cells
Known as PASTE, the technique holds potential for treating a variety of diseases caused by faulty genes.
Anne Trafton
November 24, 2022
Building on the CRISPR gene-editing system, MIT researchers have designed a new tool that can snip out faulty genes and replace them with new ones, in a safer and more efficient way.
Using this system, the researchers showed that they could deliver genes as long as 36,000 DNA base pairs to several types of human cells, as well as to liver cells in mice. The new technique, known as PASTE, could hold promise for treating diseases that are caused by defective genes with a large number of mutations, such as cystic fibrosis.
“It’s a new genetic way of potentially targeting these really hard to treat diseases,” says Omar Abudayyeh, a McGovern Fellow at MIT’s McGovern Institute for Brain Research. “We wanted to work toward what gene therapy was supposed to do at its original inception, which is to replace genes, not just correct individual mutations.”
The new tool combines the precise targeting of CRISPR-Cas9, a set of molecules originally derived from bacterial defense systems, with enzymes called integrases, which viruses use to insert their own genetic material into a bacterial genome.
“Just like CRISPR, these integrases come from the ongoing battle between bacteria and the viruses that infect them,” says Jonathan Gootenberg, also a McGovern Fellow. “It speaks to how we can keep finding an abundance of interesting and useful new tools from these natural systems.”
Gootenberg and Abudayyeh are the senior authors of the new study, which appears today in Nature Biotechnology. The lead authors of the study are MIT technical associates Matthew Yarnall and Rohan Krajeski, former MIT graduate student Eleonora Ioannidi, and MIT graduate student Cian Schmitt-Ulms.
DNA insertion
The CRISPR-Cas9 gene editing system consists of a DNA-cutting enzyme called Cas9 and a short RNA strand that guides the enzyme to a specific area of the genome, directing Cas9 where to make its cut. When Cas9 and the guide RNA targeting a disease gene are delivered into cells, a specific cut is made in the genome, and the cells’ DNA repair processes glue the cut back together, often deleting a small portion of the genome.
If a DNA template is also delivered, the cells can incorporate a corrected copy into their genomes during the repair process. However, this process requires cells to make double-stranded breaks in their DNA, which can cause chromosomal deletions or rearrangements that are harmful to cells. Another limitation is that it only works in cells that are dividing, as nondividing cells don’t have active DNA repair processes.
The MIT team wanted to develop a tool that could cut out a defective gene and replace it with a new one without inducing any double-stranded DNA breaks. To achieve this goal, they turned to a family of enzymes called integrases, which viruses called bacteriophages use to insert themselves into bacterial genomes.
For this study, the researchers focused on serine integrases, which can insert huge chunks of DNA, as large as 50,000 base pairs. These enzymes target specific genome sequences known as attachment sites, which function as “landing pads.” When they find the correct landing pad in the host genome, they bind to it and integrate their DNA payload.
In past work, scientists have found it challenging to develop these enzymes for human therapy because the landing pads are very specific, and it’s difficult to reprogram integrases to target other sites. The MIT team realized that combining these enzymes with a CRISPR-Cas9 system that inserts the correct landing site would enable easy reprogramming of the powerful insertion system.
The new tool, PASTE (Programmable Addition via Site-specific Targeting Elements), includes a Cas9 enzyme that cuts at a specific genomic site, guided by a strand of RNA that binds to that site. This allows them to target any site in the genome for insertion of the landing site, which contains 46 DNA base pairs. This insertion can be done without introducing any double-stranded breaks by adding one DNA strand first via a fused reverse transcriptase, then its complementary strand.
Once the landing site is incorporated, the integrase can come along and insert its much larger DNA payload into the genome at that site.
“We think that this is a large step toward achieving the dream of programmable insertion of DNA,” Gootenberg says. “It’s a technique that can be easily tailored both to the site that we want to integrate as well as the cargo.”
Gene replacement
In this study, the researchers showed that they could use PASTE to insert genes into several types of human cells, including liver cells, T cells, and lymphoblasts (immature white blood cells). They tested the delivery system with 13 different payload genes, including some that could be therapeutically useful, and were able to insert them into nine different locations in the genome.
In these cells, the researchers were able to insert genes with a success rate ranging from 5 to 60 percent. This approach also yielded very few unwanted “indels” (insertions or deletions) at the sites of gene integration.
“We see very few indels, and because we’re not making double-stranded breaks, you don’t have to worry about chromosomal rearrangements or large-scale chromosome arm deletions,” Abudayyeh says.
The researchers also demonstrated that they could insert genes in “humanized” livers in mice. Livers in these mice consist of about 70 percent human hepatocytes, and PASTE successfully integrated new genes into about 2.5 percent of these cells.
The DNA sequences that the researchers inserted in this study were up to 36,000 base pairs long, but they believe even longer sequences could also be used. A human gene can range from a few hundred to more than 2 million base pairs, although for therapeutic purposes only the coding sequence of the protein needs to be used, drastically reducing the size of the DNA segment that needs to be inserted into the genome.
“The ability to site-specifically make large genomic integrations is of huge value to both basic science and biotechnology studies. This toolset will, I anticipate, be very enabling for the research community,” says Prashant Mali, a professor of bioengineering at the University of California at San Diego, who was not involved in the study.
The researchers are now further exploring the possibility of using this tool as a possible way to replace the defective cystic fibrosis gene. This technique could also be useful for treating blood diseases caused by faulty genes, such as hemophilia and G6PD deficiency, or Huntington’s disease, a neurological disorder caused by a defective gene that has too many gene repeats.
The researchers have also made their genetic constructs available online for other scientists to use.
“One of the fantastic things about engineering these molecular technologies is that people can build on them, develop and apply them in ways that maybe we didn’t think of or hadn't considered,” Gootenberg says. “It’s really great to be part of that emerging community.”
Ways to connect
Telegram: @JoelWalbert
Email: thetruthaddict@tutanota.com
The Truth Addict Telegram channel
Hard Truth Soldier chat on Telegram
Mastodon: @thetruthaddict@noagendasocial.com
Session: 05e7fa1d9e7dcae8512eed0702531272de14a7f1e392591432551a336feb48357c
Odysee: TruthAddict
Donations (#Value4Value)
Bitcoin:
bc1q5jhxnkxqpc45veqd9czf2ys3th6y4ne6a96j3h (on chain)
bc1q6l4rezjv4p6vzmwmf7fkx9j5dtj3trzl3hqe048sd80su77jwq9scsy3jq (lightning)
nemesis@getalby.com
+wildviolet72C (PayNym)
Monero:
43E8i7Pzv1APDJJPEuNnQAV914RqzbNae15UKKurntVhbeTznmXr1P3GYzK9mMDnVR8C1fd8VRbzEf1iYuL3La3q7pcNmeN